Hi from ward
E39,
We are now a
few days into the chemo and it’s going to be a long and testing time for us
never mind the living hell that poor Zach is going through. His chemo schedule
consists of 4, 21 day cycles. Zach gets chemo from day 0-3, 7, 14 via his
wiggly in his side. He has 4 different chemo drugs to fight the Rb, one drug
that stops him weeing blood, as this is one of the many side effects that he
can suffer. He is also having a chemo drug put straight to the brain tumour via
the Omaya reservoir in his head. He gets this on weekdays for the first two
weeks of each cycle. This has to be done as there is a barrier called the brain
blood barrier which stops the chemo that is being administered through his
wiggly getting to his brain, this an in build safety barrier. He takes regular
calpol to help with the aching that is another side effect. He gets anti
emetics to stop him being sick, but these weren’t working very well on day 2 so
these have been changed to a drug that makes him very sleepy, which is probably
for the best as it means that he can rest and not feel rotten like he has been.
He isn’t on these all the time, just when he is at his worst. For the last
seven days of each cycle he has a rest from the chemo drugs then it all starts
again. On top of all this he will have to have stem cells harvested from his
bone marrow as the chemo drugs will “wipe out” his bone marrow. These will be
put back to help his body recover and let the stem cells in his bone marrow
re-generate before the next protocol starts. He also has to receive regular
drugs during each cycle that stop him picking up lung infections and help the
neutrophils in his blood recover.
Neutrophils help the body fight infection and are significantly reduced
after chemo is given. So if you’ve got enough fingers and toes that’s about nine
different drugs I’ve counted and I think I have missed one or two. Don’t worry
he doesn’t get every drug every day. The chemo is broken down into ones and
twos. These are often infused with large amounts of fluid so even if he isn’t
eating he is still well hydrated. The down side to this is he is going through
nappies like they are going out of fashion. We now have to be extra careful
when changing his nappies as the contents is toxic when he is receiving chemo. When
I say toxic I don’t mean they have a nasty smell, I mean skull and cross bones,
this stuff will actually cause you harm. This is because chemotherapy drugs are
cytotoxic, http://www.patient.co.uk/health/Chemotherapy.htm
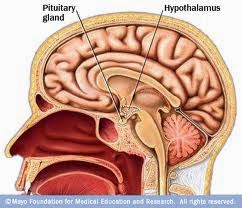
I haven’t said much about Zach’s brain
tumour so far. It is called a PNET (Primitive NeuroEctodermal Tumour), which
describes the group of tumours it belongs to and specifically it is a
Pineoblastoma. If you Google pineoblastoma there is some information it. It is
located in the third ventricle also known as the third eye, which is in the
centre of the brain (see first picture, please note this is from the internet,
not Zach but it gives you an idea). It can block the flow of Cerebral Spinal
Fluid (CSF), which is one of the reasons why he has an Omaya reservoir. This allows doctors to
remove some of the fluid if it builds up. They can also fit a shunt which is similar to an Omaya but
diverts the fluid into the abdomen. Zach doesn’t need one of these as his
tumour isn’t blocking the flow of fluid. Another option which was discussed
with us is to perform a ventriculostomy, which is where a Neurosurgeon makes a
hole in the hypothalamus to allow CSF to drain away. This would have been done
when the Omaya was being fitted and is quite routine. CSF build up is called hydrocephalus, and is quite serious. it can have symptoms that are similiar to the after effects of chemo, as we have found out.
The ward we
are on does a lot of day care so it’s busy during the week but at weekends it’s
quiet, so we can spread out a bit. Livvy our clinical nurse specialist comes to
see us a couple of times a day when she is working, so if we have questions she
can answer them or find out. She always greets us and says bye with a hug which
is reassuring. She is a very bubbly character. The prof sees us a couple of
times a week, usually with results which means of late it’s been mostly bad
news. He is a reserved man in our company, however I get the feeling when I see
him with the nurses he could be quite witty and mischievous. They have play
specialists who do as it says, play. They can take children for a wee while to
give parents/carers a break to get a cuppa. They also organise activities for
the kids to keep them occupied. Shaz a play specialist is a favourite of Zach’s
and can get a smile out of him where most others have failed including us. Our
parents have been supporting us all the way and keeping us fuelled, doing the
washing and pick up any shopping we need as well as a massive shoulder to lean
on when we need.
Another massive
thank you to all of our family and friends for the messages of support whether
they be posted on the blog or written in a card. We are somewhat amazed at how
many times the blog has been looked at. Keep the messages coming and look out
for the next post.



